Health and employment
1. For people in work, fast and convenient access to health services plays an important role in maintaining employment. Mental health and musculoskeletal conditions remain the main reason for sickness absence. NHS provision of services for both is increasing. Digital provision of mental health support is also increasing, providing more flexibility in accessing services around work. Expansion of physiotherapists working in primary care networks will be one way in which patients will see the right professional first time. People who are off work for more than four weeks are more likely to fall out of work permanently. Personalised care plans that support people to manage their condition in work, with reasonable adjustments where needed, will reduce this.
Figure 29: Percentage of the population who are employed, by disability status, England, 2016 to 2017.
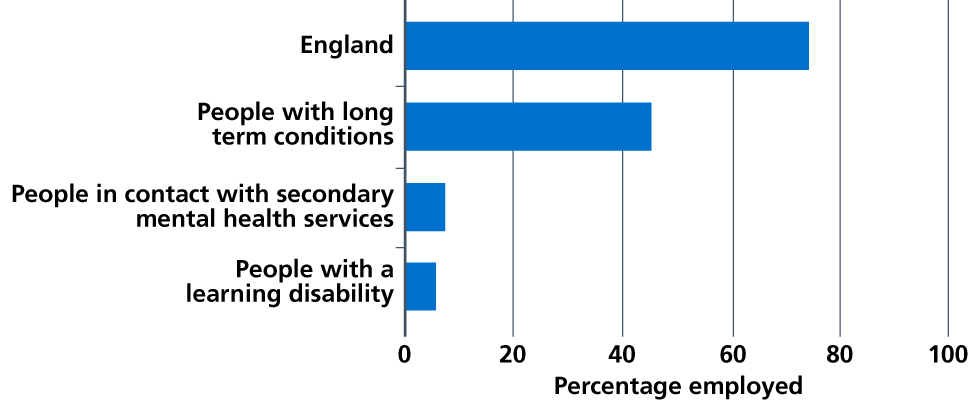
Source: Public Health England. Health profile for England: 2018. September 2018.
2. Stable employment is a major factor in maintaining good mental health, and is an important outcome for recovery for people with a mental health problem. For people being supported by secondary mental health services, there is a 65% employment gap compared with the general population. And people with mental health problems are also often over-represented in high-turnover, low-pay and often part-time or temporary work.
3. The NHS is on track to support up to 20,000 people with severe mental illness to find and retain employment by 2020/21. Based on over 20 years of research, the Individual Placement and Support (IPS) employment model is internationally recognised as the most effective way to support people with mental health problems to gain and keep paid employment. On average, people who receive IPS show employment rates of 30-40% compared to rates in the control group of 10-12%. Those supported by IPS work significantly more hours per month, and have higher earnings and better job tenure. Some show reduced rates of hospital admission and less time spent in hospital. Follow-up studies over 8-12 years confirm these better outcomes are maintained over the longer term. These schemes have also been shown to be cost-effective.
4. In May 2018, with the government, Sheffield City Region and the West Midlands Combined Authority, the NHS launched the world’s largest trial of IPS services. This trial is evaluating whether IPS can be equally as valuable and cost effective for people who have any health condition and are using primary and community care services. A trial providing employment support via IAPT will also offer support to 24,000 people by 2021. Where these health and work trials are effective, the NHS will work with government to secure investment for future provision.
5. Through increasing access to IPS, the NHS will support an additional 35,000 people with severe mental illnesses where this is a personal goal to find and retain employment by 2023/24, a total of 55,000 people per year. This investment will support people to get back into or gain access to employment. It will improve outcomes and recovery for people, meaning they spend less time in hospital and live healthier, happier lives. By 2028/29, we aim to extend this to 50% of the eligible population to benefit up to 115,000 people.
6. We will continue to offer more opportunities for people with a learning disability and for people with autism. Supported internship opportunities targeted at people with a learning disability and/or autism will increase by 2023/24, with at least half converted to paid employment over the first five years of the Long Term Plan. The number of NHS internship and employment programmes/sites delivered through ‘Project Search’ and ‘Project Choice’ will increase as will the number of NHS organisations making the Learning Disability Employment Programme pledge.
7. Employers have a key role to play in supporting their staff to stay well and in work. The government has published a framework to help employers record and voluntarily report information on disability, mental health and wellbeing in the workplace [185]. The framework invites employers to report on training and support provided to staff, uptake of support, recruitment and retention rates and results from staff surveys. It also links in recommendations from Thriving at Work and Disability Confident. This framework sits alongside the Campaign to End Loneliness pledge that asks employers to commit to supporting their employees’ social wellbeing. There is still more to do and we welcome the government’s commitment to consulting on measures to encourage and support all employers to play their part in this agenda and to improve access to occupational health.
8. Sickness absence rates in the NHS are higher (4% in 2017) than other public sector organisations (2.9% in 2016) and the private sector (1.9% in 2016) [186]. Our new Chief People Officer will lead work to improve our staff health and wellbeing, and help close this gap to the public sector average. Building on existing work with 70 organisations, we will provide targeted support to trusts to access fast track occupational health services and a line management development programme. This complements the recent publication of the NHS Health and Wellbeing Framework [187], which includes recommendations from Thriving at Work: The Stevenson/Farmer review of mental health and employers [188].
References
185. Department for Work and Pensions & Department of Health and Social Care (2018) Voluntary reporting on disability, mental health and wellbeing. Available from: https://www.gov.uk/government/publications/ voluntary-reporting-on-disability-mental-health-and-wellbeing
186. Office of National Statistics (2017) Sickness absence in the UK labour market: 2016. Available from: https://www.ons.gov.uk/employmentandlabourmarket/peopleinwork/labourproductivity/articles/ sicknessabsenceinthelabourmarket/2016
187. NHS Employers (2018) NHS Health and Wellbeing Framework. Available from: https://www.nhsemployers.org/ case-studies-and-resources/2018/05/nhs-health-and-wellbeing-framework
188. Department for Work and Pensions & Department of Health and Social Care (2017) Thriving at Work: the Stevenson/Farmer review of mental health and employers. Available from: https://www.gov.uk/government/ publications/thriving-at-work-a-review-of-mental-health-and-employers
